Summer 2017 GP Newsletter
Herpes Simplex or HSV keratitis is a common cause of red eye in a broad range of age groups including children, as well as the elderly. Most commonly, it affects one eye, but can be bilateral in 10% of cases. It is most commonly due to HSV-1.
After primary infection, the herpes simplex virus remains dormant in the trigeminal ganglion. It replicates there and travels down branches of the trigeminal nerve during periods of reactivation. Involvement of the first (ophthalmic) branch of the trigeminal nerve results in ocular herpes disease.
Ocular herpes simplex disease can involve the eye lids and conjunctiva (blepharoconjunctivitis), the cornea (keratitis), as well the internal structures of the eye, including iritis, retinitis, and optic neuritis, the latter two being quite rare.
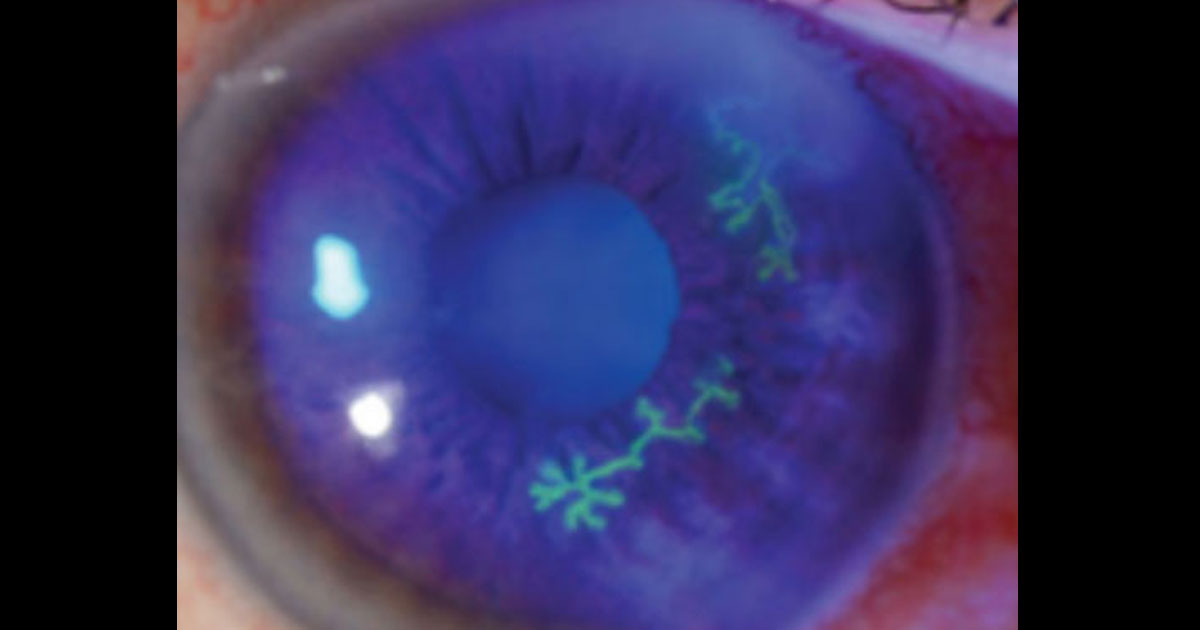
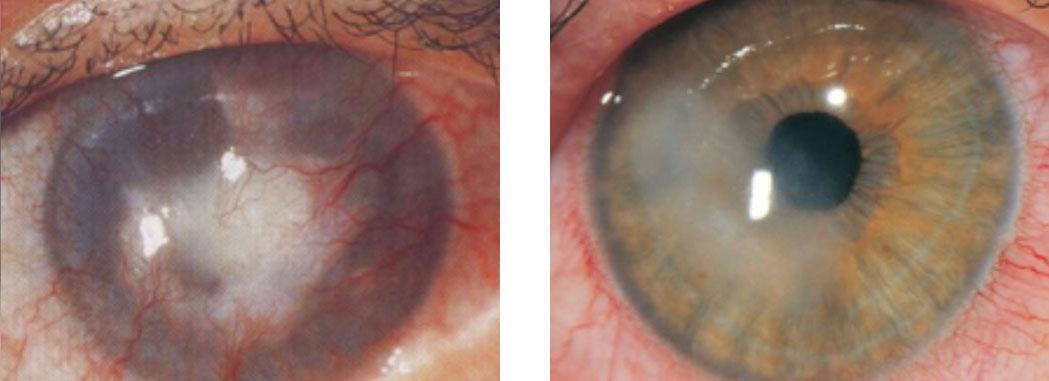
Involvement of the cornea (keratitis) is the commonest manifestation of ocular herpes disease. The keratitis may be due to direct viral invasion with a classic branching (‘dendritic’) corneal ulcer (above image), or it may an immune-mediated and affect the deeper layers of the cornea. Two forms of the immune-mediated keratitis are shown below. The image on the left demonstrates stromal keratitis and corneal neovasculisation, and the image on the right demonstrates endothelial keratitis and an overlying area of corneal oedema.
After primary infection, the herpes simplex virus remains dormant in the trigeminal ganglion. It replicates there and travels down branches of the trigeminal nerve during periods of reactivation. Involvement of the first (ophthalmic) branch of the trigeminal nerve results in ocular herpes disease.
Ocular herpes simplex disease can involve the eye lids and conjunctiva (blepharoconjunctivitis), the cornea (keratitis), as well the internal structures of the eye, including iritis, retinitis, and optic neuritis, the latter two being quite rare.
Involvement of the cornea (keratitis) is the commonest manifestation of ocular herpes disease. The keratitis may be due to direct viral invasion with a classic branching (‘dendritic’) corneal ulcer (above image), or it may an immune-mediated and affect the deeper layers of the cornea. Two forms of the immune-mediated keratitis are shown below. The image on the left demonstrates stromal keratitis and corneal neovasculisation, and the image on the right demonstrates endothelial keratitis and an overlying area of corneal oedema.
The typical symptoms of herpes simplex keratitis include foreign-body sensation, photophobia, tearing, redness, and blurred vision. Unlike bacterial keratitis or iritis, eye pain is NOT a significant feature of this disease due to the neurotrophic properties of the virus. Repeated episodes of herpes keratitis permanently affects corneal innervation. These nerves are crucial to the maintenance of corneal health and lubrication. Such patients in the long-term develop a severe and unilateral dry eye with spontaneous breakdown of the corneal surface and poor healing.
The general practitioner could easily diagnose the dendritic form of the corneal disease with the use of topical fluorescein and cobalt blue light. Generally speaking, an ophthalmologist is best placed to diagnose the immune-mediated forms of herpes keratitis, which differ slightly in their treatment, and often require extended periods of topical steroid use.
The mainstay of treatment is antivirals (e.g. acyclovir, valaciclovir) +/- topical steroids. Occasionally, patients may need to remain on low dose oral antivirals long-term to reduce recurrence risk. Whilst topical antivirals (e.g. Zovirax ophthalmic ointment) may be initiated by the GP for dendritic keratitis, it should not be used for more than 1 week because it is toxic to the cornea. Most patients therefore require expedited review by an ophthalmologist for consideration of oral antivirals and topical steroids.
The general practitioner could easily diagnose the dendritic form of the corneal disease with the use of topical fluorescein and cobalt blue light. Generally speaking, an ophthalmologist is best placed to diagnose the immune-mediated forms of herpes keratitis, which differ slightly in their treatment, and often require extended periods of topical steroid use.
The mainstay of treatment is antivirals (e.g. acyclovir, valaciclovir) +/- topical steroids. Occasionally, patients may need to remain on low dose oral antivirals long-term to reduce recurrence risk. Whilst topical antivirals (e.g. Zovirax ophthalmic ointment) may be initiated by the GP for dendritic keratitis, it should not be used for more than 1 week because it is toxic to the cornea. Most patients therefore require expedited review by an ophthalmologist for consideration of oral antivirals and topical steroids.
