Spring 2016 GP Newsletter
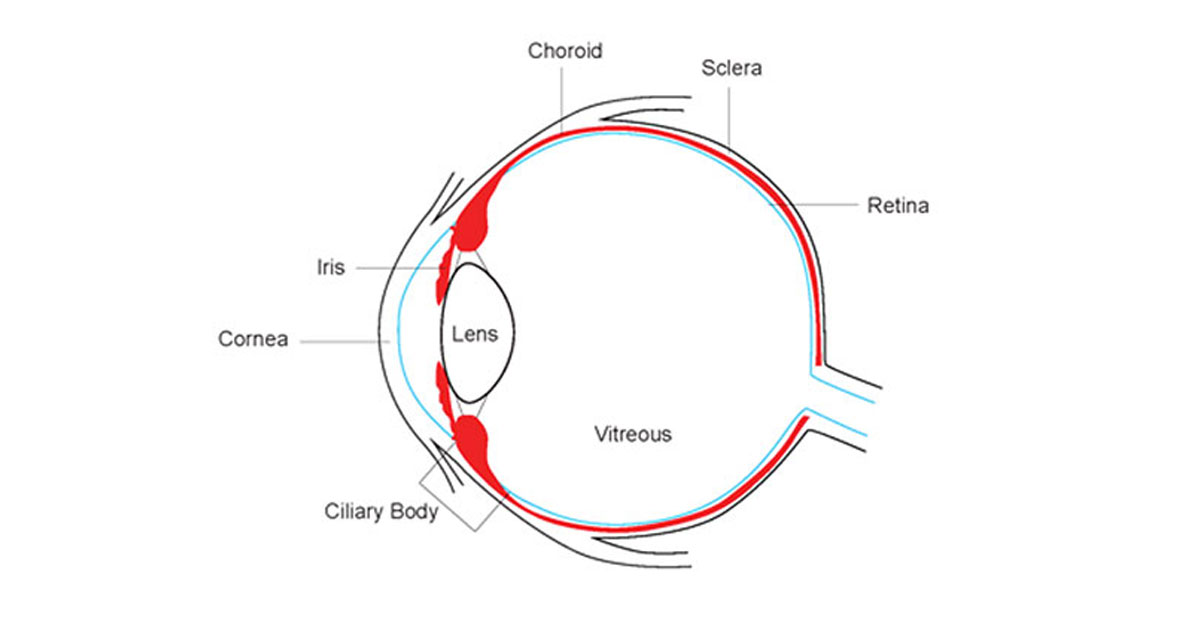
The uveal tract is the pigmented middle coat of the eye, consisting of the iris, ciliary body and choroid. Uveitis is the inflammation of any part of the uveal tract, and panuveitis refers to inflammation of all three areas.
Anterior uveitis (iritis) accounts for the vast majority of uveitis seen in primary care. It usually, but not always, affects only one eye.
1. Aetiology
In 50% of cases, iritis is idiopathic. The remainder are associated with seronegative spondyloarthropathies (most commonly ankylosing spondylitis), infections (e.g. herpes simplex, herpes zoster, and syphilis), autoimmune conditions (e.g. sarcoidosis), and several rarer conditions. In children, juvenile idiopathic arthritis is a notable association.
2. Clinical features
Iritis tends to affect young to middle-aged adults. Older patients tend to have an underlying cause, rather than idiopathic aetiology.
Symptoms include eye and periorbital pain, redness that is most prominent around the corneal limbus (‘ciliary flush’ – Figure 2), photophobia and possibly reduced vision. Patients may report prior episodes.
Anterior uveitis (iritis) accounts for the vast majority of uveitis seen in primary care. It usually, but not always, affects only one eye.
1. Aetiology
In 50% of cases, iritis is idiopathic. The remainder are associated with seronegative spondyloarthropathies (most commonly ankylosing spondylitis), infections (e.g. herpes simplex, herpes zoster, and syphilis), autoimmune conditions (e.g. sarcoidosis), and several rarer conditions. In children, juvenile idiopathic arthritis is a notable association.
2. Clinical features
Iritis tends to affect young to middle-aged adults. Older patients tend to have an underlying cause, rather than idiopathic aetiology.
Symptoms include eye and periorbital pain, redness that is most prominent around the corneal limbus (‘ciliary flush’ – Figure 2), photophobia and possibly reduced vision. Patients may report prior episodes.

Figure 2 – Perilimbal injection (‘ciliary flush’)
It is important that any patient presenting with any of the above symptoms not be mistakenly diagnosed with ‘conjunctivitis’. Typically, significant eye pain, photophobia and reduced vision are not features of conjunctivitis.
The creation of posterior synechiae is one of the complications of iritis. These are adhesions between the anterior surface of the lens capsule and the iris.
The creation of posterior synechiae is one of the complications of iritis. These are adhesions between the anterior surface of the lens capsule and the iris.
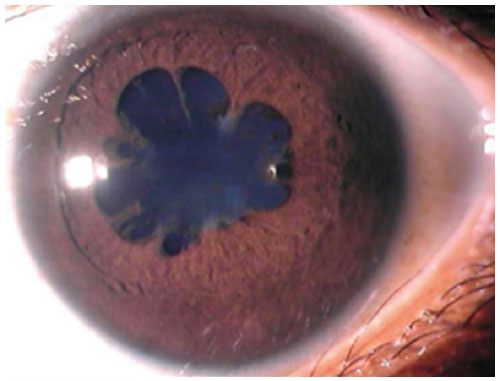
Figure 3 – Posterior synechiae (iris adhesions to lens)
If extensive they may impede the normal flow of aqueous, thus raising the intraocular pressure.
3. Management
Within the primary care setting, the GP's role is to consider the diagnosis of iritis and refer appropriately. All patients with a painful red eye, with altered vision or photophobia without an adequate explanation should be referred to an ophthalmologist, and ideally be seen the same day.
Dilating the pupil by application of eye drops, such as tropicamide, helps reduce the formation of posterior synechiae. Intensive topical steroids are the mainstay of treatment. If the therapeutic response is poor, a periocular injection of steroids or even oral prednisone may be used. Rarely, patients require steroid sparing agents such as methotrexate, and these patients are best co-managed by their GP and an immunologist, as well as their ophthalmologist.
Please remember that regular topical steroid use can lead to cataract and glaucoma, as well as reducing the cornea’s immunity to herpetic and bacterial infections. With this in mind, patients should be discouraged from self-treating recurrent iritis with topical steroids in an unsupervised manner.
3. Management
Within the primary care setting, the GP's role is to consider the diagnosis of iritis and refer appropriately. All patients with a painful red eye, with altered vision or photophobia without an adequate explanation should be referred to an ophthalmologist, and ideally be seen the same day.
Dilating the pupil by application of eye drops, such as tropicamide, helps reduce the formation of posterior synechiae. Intensive topical steroids are the mainstay of treatment. If the therapeutic response is poor, a periocular injection of steroids or even oral prednisone may be used. Rarely, patients require steroid sparing agents such as methotrexate, and these patients are best co-managed by their GP and an immunologist, as well as their ophthalmologist.
Please remember that regular topical steroid use can lead to cataract and glaucoma, as well as reducing the cornea’s immunity to herpetic and bacterial infections. With this in mind, patients should be discouraged from self-treating recurrent iritis with topical steroids in an unsupervised manner.
