
Herpes Zoster Ophthalmicus
Herpes Zoster Ophthalmicus (HZO) is defined by involvement of the ophthalmic branch of the trigeminal nerve (CN V1). This branch supplies the forehead, the anterior scalp, the side and tip of the nose, ethmoidal sinuses, and importantly, all structures within the globe, including the retina and optic nerve. Zoster involving the maxillary division of the trigeminal nerve (CN V2) is not globe threatening, and does not require referral to an ophthalmologist.
The classic vesicular rash can result in significant upper facial oedema, which is often misdiagnosed as periorbital cellulitis. Secondary bacterial infection involving the eyelids is actually quite uncommon, and systemic antibiotics are seldom required.
HZO accounts for 10-20% of all cases of shingles, with ocular involvement in up to 50%, so referral to an ophthalmologist is recommended within a week. Prompt commencement of oral antivirals (valaciclovir, famciclovir, or acyclovir) alters the disease course favourably. All three have comparable efficacies in the treatment of HZO, particularly in terms of resolution of acute pain, rash, viral shedding, and ocular complications. Although acyclovir is inferior to the other two in reducing the incidence, severity and duration of post-herpetic neuralgia (PHN).
The earliest form of ocular involvement is conjunctivitis or episcleritis, both are benign and self-limiting. Scleritis, an exquisitely painful condition and a far more serious complication, can also occur early, and result in patchy scleral atrophy later on. Fortunately, it is rare.
HZO can result in multiple corneal complications, which are all fairly common. Some are directly due to the virus, whilst others are immune-mediated or due to anterior segment vasculitis or neuropathy. Neurotrophic corneal problems can occur abruptly months after an episode of HZO, resulting in diminished corneal sensation and chronic ocular surface problems.
Another common complication of HZO is anterior uveitis, which usually occurs 2-3 weeks after the initial rash, but can become chronic and be associated with raised intraocular pressure.
The classic vesicular rash can result in significant upper facial oedema, which is often misdiagnosed as periorbital cellulitis. Secondary bacterial infection involving the eyelids is actually quite uncommon, and systemic antibiotics are seldom required.
HZO accounts for 10-20% of all cases of shingles, with ocular involvement in up to 50%, so referral to an ophthalmologist is recommended within a week. Prompt commencement of oral antivirals (valaciclovir, famciclovir, or acyclovir) alters the disease course favourably. All three have comparable efficacies in the treatment of HZO, particularly in terms of resolution of acute pain, rash, viral shedding, and ocular complications. Although acyclovir is inferior to the other two in reducing the incidence, severity and duration of post-herpetic neuralgia (PHN).
The earliest form of ocular involvement is conjunctivitis or episcleritis, both are benign and self-limiting. Scleritis, an exquisitely painful condition and a far more serious complication, can also occur early, and result in patchy scleral atrophy later on. Fortunately, it is rare.
HZO can result in multiple corneal complications, which are all fairly common. Some are directly due to the virus, whilst others are immune-mediated or due to anterior segment vasculitis or neuropathy. Neurotrophic corneal problems can occur abruptly months after an episode of HZO, resulting in diminished corneal sensation and chronic ocular surface problems.
Another common complication of HZO is anterior uveitis, which usually occurs 2-3 weeks after the initial rash, but can become chronic and be associated with raised intraocular pressure.
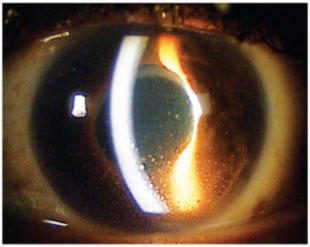
Anterior uveitis due to HZO. Deposits of white blood cells can be seen on the inner aspect of the cornea inferiorly.
Fortunately the posterior segment complications of herpes zoster are uncommon, but can be devastating. Optic neuritis can result in permanent loss of vision, and acute retinal necrosis can cause widespread retinal damage.
Ocular motor palsies resulting in diplopia are also common in the acute phase, and can involve the 3rd, 4th, or 6th cranial nerves. Oral corticosteroids should be considered for this subgroup. Oral steroids also play a beneficial role in management of patients with severe rash or severe pain that is not controlled by opioids. There is good evidence to suggest that prednisone accelerates skin healing and resolution of acute pain, and helps improve motor outcomes in those with ocular motor palsies.
Ocular motor palsies resulting in diplopia are also common in the acute phase, and can involve the 3rd, 4th, or 6th cranial nerves. Oral corticosteroids should be considered for this subgroup. Oral steroids also play a beneficial role in management of patients with severe rash or severe pain that is not controlled by opioids. There is good evidence to suggest that prednisone accelerates skin healing and resolution of acute pain, and helps improve motor outcomes in those with ocular motor palsies.
